How Aging Affects the Digestive System
The digestive tract includes the esophagus, stomach, small and large intestines, liver, pancreas, and gallbladder. Each of these components can be affected by aging in different ways. Here’s how:
1. Slower Gastrointestinal Motility
One of the most noticeable age-related changes is a slower movement of food through the digestive tract. This can lead to constipation, bloating, and discomfort.
2. Decreased Production of Digestive Enzymes
With age, the stomach produces less hydrochloric acid (HCl) and other digestive enzymes. This hampers the breakdown of food and absorption of nutrients like Vitamin B12, calcium, and iron.
3. Changes in Gut Microbiota
The gut houses trillions of beneficial bacteria. Aging can reduce bacterial diversity, contributing to gut inflammation, a weakened immune system, and digestive disorders.
4. Weakened Muscles in the Digestive Tract
The muscles that line the digestive organs may lose tone and strength, slowing down digestion and making bowel movements more difficult.
5. Reduced Liver and Pancreatic Function
Age may impair the liver’s ability to detoxify the blood and reduce the pancreas’s enzyme output, affecting nutrient metabolism and increasing the risk of diabetes.
There are many changes that come with aging, some little and some more noticeable. While it is common knowledge that wrinkles, gray hair, and low energy are common, gut health is one area that is frequently disregarded. Our digestive tract changes physiologically and functionally as we age, which can have a big effect on our general health. Constipation, acid reflux, delayed digestion, and decreased nutrient absorption are among the problems that older adults may encounter.
Maintaining ideal digestive function and avoiding gastrointestinal diseases later in life depend on an understanding of these changes. This article discusses the effects of aging on the digestive system, typical warning signs, and how older adults can maintain gut health.
Common Digestive Problems in Seniors

Here are the most prevalent digestive issues faced by older adults:
1. Constipation
Due to reduced motility, inadequate fluid intake, poor diet, or medications, constipation is a widespread problem among seniors.
2. Gastroesophageal Reflux Disease (GERD)
Weakened esophageal sphincter muscles can lead to acid reflux, heartburn, and GERD.
3. Peptic Ulcers and Gastritis
Use of NSAIDs, alcohol, or H. pylori infection can cause inflammation of the stomach lining or ulcers.
4. Lactose Intolerance
The body may produce less lactase enzyme over time, making it difficult to digest dairy products.
5. Diverticulosis
With age, the walls of the colon may develop small pouches called diverticula, which can become infected or inflamed.
6. Malabsorption and Nutrient Deficiency
Poor enzyme production and lower stomach acid can lead to deficiencies in vitamins B12, D, iron, and calcium.
7. Gallstones
Gallbladder function declines with age, increasing the risk of gallstones and bile duct obstruction.
The Gut-Brain Connection in Seniors

The gut-brain axis plays a crucial role in mental and emotional well-being. Poor gut health in seniors has been linked to cognitive decline, depression, and mood disorders. This is partly due to decreased microbial diversity and chronic low-grade inflammation.
Maintaining a healthy gut may help reduce brain fog, enhance memory, and support emotional stability in older adults.
Diet and Lifestyle Tips to Support Digestive Health in Seniors
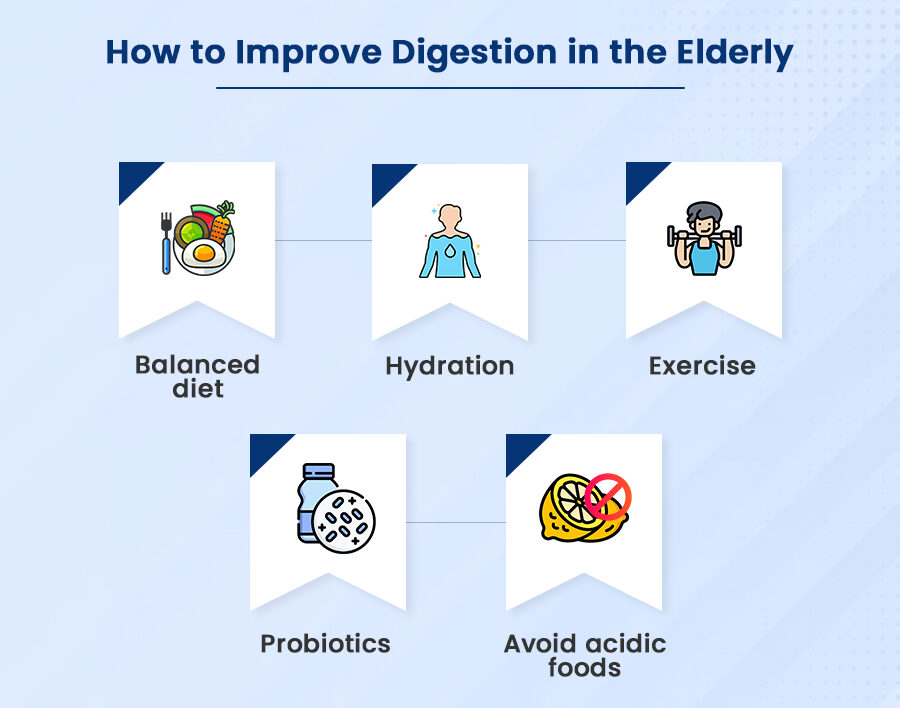
1. Eat a High-Fiber Diet
Fiber promotes regular bowel movements and prevents constipation. Include:
Whole grains
Fresh fruits and vegetables
Legumes
Nuts and seeds
2. Stay Hydrated
Older adults often have a reduced sense of thirst, making dehydration more common. Drink at least 6–8 glasses of water a day.
3. Eat Smaller, Frequent Meals
This approach reduces strain on the digestive system and helps in better nutrient absorption.
4. Limit Fatty and Fried Foods
These can slow digestion and worsen GERD symptoms.
5. Avoid Processed Sugars and Refined Carbs
They disrupt gut flora and contribute to bloating and inflammation.
6. Consume Probiotic-Rich Foods
Yogurt, kefir, kimchi, sauerkraut, and kombucha can help replenish good gut bacteria.
7. Moderate Alcohol and Caffeine
Both can irritate the stomach lining and contribute to acid reflux or gastritis.
8. Exercise Regularly
Gentle exercise like walking or yoga stimulates bowel movements and improves overall digestion.
Medication and Its Role in Digestive Issues
Many older adults take medications for chronic conditions like diabetes, hypertension, or arthritis. However, several commonly prescribed drugs can interfere with digestion, including:
NSAIDs: Can cause ulcers or gastritis
Calcium channel blockers: May lead to constipation
Iron supplements: Can cause stomach upset
Antibiotics: Disrupt gut bacteria
It’s essential to review medications regularly with a healthcare provider to avoid digestive complications.
When to See a Doctor
Not all digestive issues in seniors are age-related. Seek medical attention if any of the following symptoms persist:
Unexplained weight loss
Blood in stools
Chronic constipation or diarrhea
Difficulty swallowing
Severe abdominal pain
Nausea or vomiting lasting more than a few days
These symptoms may signal serious conditions like colorectal cancer, ulcers, or gastrointestinal infections.
Natural Remedies and Supplements
1. Psyllium Husk or Isabgol
A natural fiber that helps relieve constipation.
2. Digestive Enzyme Supplements
Especially beneficial if enzyme production is low due to aging.
3. Probiotics
Available in capsule or powder form to improve gut flora.
4. Herbal Teas
Peppermint, fennel, and ginger teas are excellent for relieving bloating and indigestion.
Note: Always consult a healthcare provider before starting supplements.
Preventive Health Screenings for Seniors
Regular screenings help detect issues early. Seniors should consider:
Colonoscopy (every 10 years after age 50)
Stool tests (for blood or infection)
Nutrient level checks (B12, D, iron)
Bone density tests (calcium absorption issues can affect bones)
Special Considerations for Seniors in Assisted Living
Seniors in care homes or assisted living facilities often experience more digestive issues due to:
Sedentary lifestyle
Institutional diets low in fiber
Limited hydration
Polypharmacy (multiple medications)
Caregivers must be educated about digestive needs and ensure:
Adequate fiber and fluid intake
Regular physical activity
Prompt attention to gastrointestinal complaints
My Opinion: Digestive Health is Vital for Healthy Aging
As the saying goes, “You are what you digest.” In seniors, digestive health is not just about comfort—it’s deeply connected to immunity, mental well-being, and longevity.
By being proactive with diet, lifestyle, and routine checkups, older adults can manage age-related digestive changes effectively. Family members and caregivers should also be aware of these changes and support seniors in maintaining a gut-friendly routine.
Investing in digestive wellness is a powerful step toward graceful and healthy aging.
Related posts:
 Sustainable Living: Small Changes That Make a Big Impact
Sustainable Living: Small Changes That Make a Big Impact
 Embracing the Tranquility: A Guide to Finding Full Relaxation on a Rainy Day
Embracing the Tranquility: A Guide to Finding Full Relaxation on a Rainy Day
 Benefits of Aerobic Exercise for Cardiovascular Health
Benefits of Aerobic Exercise for Cardiovascular Health
 Unlocking the Secrets of Sleep: How Sleep Physiology Shapes Brain Function
Unlocking the Secrets of Sleep: How Sleep Physiology Shapes Brain Function
 Mind and Body Balance: A Holistic Approach to Health, Happiness, and Success
Mind and Body Balance: A Holistic Approach to Health, Happiness, and Success
 How Stress Affects Digestion – Gut Health & Mental Wellness Connection
How Stress Affects Digestion – Gut Health & Mental Wellness Connection
